Understanding the Term Referred Pain
PAIN THAT MOVES –
A BLOG ABOUT ‘REFERRED PAIN’ AND HOW IT WORKS
We often have patients complaining of neck and back pains that refer to different areas such as their arms or legs; when pain caused by one area of the body is felt in a different location this is called referred pain. For example, one time Joe told me that he injured his back at the gym and was starting to feel pain in his groin now, and I said “Hmm, that sounds like L1-2”. Needless to say Joe’s face wore an expression of bewilderment.
Sorry Joe! Here’s what I then continued to say; “Joe, the discs in between your spinal joints usually put up with a lot of loading forces. Sometimes, the loads are too high and this causes the discs to ooze out a bit. On some occasions, the nerve roots that exit through the spinal joints get affected by inflammation around the injury or by the hernia itself. Specific parts of the skin and muscles in your legs are supplied by nerves that come out at different levels in your spine. That could be why you are experiencing the pain in your groin. We’ll have to assess your back a bit further to confirm this though.”
LAYMENS LINGO FOR REFERRED PAIN
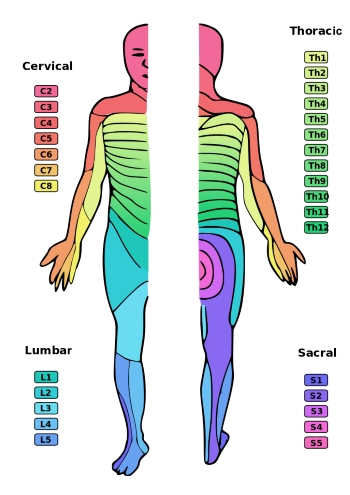
Here’s a less abridged version of what I said to Joe. Nerve roots that exit at the spinal cord have a sensory component and a motor (related to movement) component. Dermatomes are an area of skin supplied by a specific nerve root. Myotomes are groups of muscle supplied by a single nerve root. The pictures below will help you understand this one a bit better.
In Joe’s case, the L1 and L2 nerve roots may have been affected by the injury to his disc. These nerve roots are responsible for innervating the skin of the groin area as well as some of the muscles around the hip.
Therefore, Joe might be experiencing some sensory changes in his groin such as pain or pins and needles. He might also experience weakness in some hip muscles.
Similarly, if a patient, Mrs. X tells me that her pain started at the back and is referring down into her calf, I’d be thinking about the possibility of the L5-S1 nerve roots being affected down lower into the lumbar spine. This type of pain, where there is direct injury to a nerve is called neuropathic pain.
Mrs. X’s particular condition is referred to as sciatica is only diagnosed if there is a pathology affecting the sciatic nerve itself (which arises from the nerve roots L3, L4, L5, S1, S2 and S3). This can occur due to lumbar or sacral disc herniations, spinal tumours, spinal stenosis (narrowing of the spinal cord) or due to ‘piriformis syndrome’.
WHAT IS THE PIRIFORMIS SYNDROME?
The Piriformis syndrome is a condition that causes compression of the sciatic nerve due to overuse or tension in the piriformis muscle of the buttock.
In approximately 15% of people, the sciatic nerve runs through the muscle rather than underneath it. Such unfortunate people are more likely to develop sciatica. More often than not, sciatica is over-diagnosed.
This is because similar symptoms can occur with the presence of trigger points in the lower back and buttock. Another mechanism by which people might present with these lower limb symptoms is when the pain is referred in a dermatomal pattern without direct injury to the nerve. The mechanism of this process however, is unclear.
HOW CAN A PHYSIOTHERAPIST HELP WITH REFERRED PAIN?
When patients present at our clinic with complaints of back and neck pain with referred symptoms, it takes a physical therapist with a broad knowledge of anatomy and pain mechanisms to accurately diagnose the condition. The history we get from you, the patient, determines the kind of testing you undergo. In some cases your physiotherapist may choose to test specific dermatomes with a sensory test or your myotomes by checking muscle strength and reflexes. In more complex cases, it may be necessary to refer to an MRI for a more specific diagnosis.
Regardless of the complexity of the condition, it is important to realise that pain shouldn’t be ignored. Even the smallest niggle can turn into moderate pain if left unattended. If there is one thing you learn as a physiotherapist, it is that you do not want an acute condition to turn into a chronic one. Chronic pain mechanisms are very different to that of acute pain and can be very detrimental to your quality of life, not to mention, much harder to treat; but that’s a story for another blog. My advice to you is to seek assistance from a physiotherapist or exercise physiologist if you injure yourself before your pain turns into a chronic condition.
Have more questions? Reach out to one of our expert physio Brisbane team members and they will help answer your questions. Call today on 07 3352 5116 to make an appointment or make a booking online.
UPDATED 17/06/2022







