The Ultimate Plantar Fasciitis Treatment Guide
The Ultimate Plantar Fasciitis Treatment Guide
| Plantar Fasciitis can cause severe foot pain. If you live in Newmarket, Windsor, Wilston, Red Hill, Kelvin Grove or Ashgrove. Call Us today. |
By James Speck via Somastruct.
I’ve both had plantar fasciitis myself and have regularly treated patients with the condition. I’ve seen a lot of confusing information presented about how to treat plantar fasciitis. Most commonly recommended treatments are generally ineffective, can be costly, and more often than not fail to provide heel pain sufferers with permanent relief.
Effective treatment requires treating the cause and not just the symptoms of heel pain. This article outlines a step-by-step plan based on the current understanding of how plantar fasciitis develops.
This is Part 3 in a three-part series on Plantar Fasciitis.
- Part 1: The Real Cause of Plantar Fasciitis
- Part 2: Why Common Treatments Don’t Work
- Part 3: Treatment Guide for Plantar Fasciitis
Part 1 discussed the factors I think can likely contribute to plantar fasciitis.
Part 2 reviewed the lack of effectiveness of conventional treatment approaches such as arch supports, cortisone injections, and night splints.
Common Misconceptions About Plantar Fasciitis
- It is not caused by wearing shoes that don’t have enough support
- It is not caused by a tight plantar fascia
- It is not caused by running, or spending a lot of time on your feet

Things To Know About Heel Pain
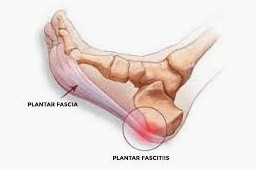
Plantar fasciitis is a painful condition characterized by a gradual onset of pain on the bottom of the heel near the inside of the foot. The pain is usually the most intense with the first steps in the morning or after periods of inactivity.
The plantar fascia is a thick band on the bottom of the foot, running from the toes to the heel. Deep to the fascia there are muscles that also span the length of the foot and insert on the heel in the same area as the plantar fascia. Together, these structures provide support to the foot and aid in shock absorption.
Possible contributing factors to the development of plantar fasciitis:
- Compression on the heel leading to increased load and reduced circulation
- Footwear that alters the normal function of the foot
- Weakness of the foot muscles that transfers load to the plantar fascia
- Abnormal stress on the arch from decreased ankle flexibility, pronation, or a high BMI
Goals of Plantar Fasciitis Treatment
Effective treatment of plantar fasciitis likely involves replacing abnormal stress on foot with healthy stress that will promote tissue regeneration. This approach involves:
- Reducing Compression
- Increasing Circulation
- Increasing Flexibility
- Increasing Foot Strength

Plantar Fasciitis Treatment Guide
Below is an outline of the approach used for plantar heel pain. The steps involved are:
- Changing standing posture and habits to take pressure off your heel
- Increase barefoot activity
- Increase ankle flexibility
- Wearing flat, less supportive shoes
- Strengthening the muscles in the foot and leg
- Stretching and massage for the legs and feet
Step 1: Shift Weight Off The Heels
When standing, shifting weight forward to balance weight evenly between the front (ball) of the foot and heel relieves compression under the heel. Shifting weight forward also potentially increases circulation to the heel. Injured tissue needs a good blood supply to repair itself.
Taking weight off the heel and placing it more on the forefoot also allows the toes and the front of the foot to engage the ground. This activates the muscles that run along the bottom of the foot and attach on the heel bone. Increasing the strength of these muscles may be one of the key components of treating the condition.
For walking, concentrating on pushing off with the back foot instead of reaching out and landing with a hard heel strike on the front leg may also alter the stresses on the foot in a beneficial way.
Step 2: Increase Barefoot Activity
Many of us spend most of our time walking around in shoes on perfectly flat surfaces. The foot is capable of bending and twisting in many different ways. This flexibility allows the foot to conform to whatever surface we are walking on. There are also many muscles that allow the foot to make quick adjustments, as well as sensory receptors that continuously supply information to the brain.
Always walking in shoes, or spending too much time on hard, flat surfaces limits these actions of the foot. Walking barefoot as much as possible, and on as many different surfaces can help change this. Grass, dirt, sand etc. Walking barefoot can also be used as a tool to learn to land softer, with a less impact forces when the foot strikes the ground.

Step 3: Increase Ankle Flexibility
A lack of ankle flexibility is one of the most reliable risk factors for developing plantar fasciitis. Decreased ankle dorsiflexion range of motion alters the mechanics of the foot and can cause abnormal forces under the heel.
There are several ways to stretch your calves, but one of my favorites is simply walking up a steep hill. It’s simple and effective. The ancient Greek physician Hippocrates said, “walking is man’s best medicine”.
In terms of specific calf stretching exercises, there are lots of option. Two common ones are:
- Runner’s Stretch
- Soleus Stretch
Runner’s Stretch
Lean against a wall with the leg to be stretched in back. Keep the heel down and the back knee straight, lean forward until a stretch is felt in the calf.
Soleus Stretch
A similar position to the runner’s stretch, except this time the leg in front will be the one getting stretched. Keeping the heel of the leg in front flat, lean into the wall while bending the front knee until a stretch is felt in the back of that leg.
These exercises look similar but both are important because they target different muscle groups. There are two keys to making these ankle stretching exercises effective:
- Keep the feet pointed straight ahead
- Don’t let the arch collapse
Step 4: Change Shoes
I’d like to dispel the myth that the foot needs support 24/7. I suspect shoes are in many cases the culprit behind plantar fasciitis. Not because they don’t support the foot, but rather because they often give too much support!
Muscles and connective tissue need movement and activity to remain healthy. At the time I developed plantar fasciitis I was wearing stability running shoes with insoles everyday for 8-9 hours. The heel pain went away a short time after I switched to more flexible shoes with less arch support.
Understand that there is very little scientific evidence showing the stability features in shoes help prevent or treat injuries. There is no one size fits all approach to selecting shoes, but the features I consider important are:
- Flexible Sole
- Little or No Support
- Minimal Toe Spring
- Flat or Low Heel Height

Flexible Sole
I prefer shoes that are capable of bending along the entire length of the sole. This can be tested by bending and twisting the shoe.
A sole that is too stiff or one that only bends in certain spots is going to force the foot to conform to the motion of the shoe when really it should be the other way around. The shoe should match the motion of the foot and this is only going to happen in a flexible shoe.
Minimal Toe Spring
Take a look at Part 1 for an in-depth review of the effect a toe spring has on the foot. Basically, the toe spring keeps the toes elevated off the ground for the majority of the time when standing or walking. This alters the normally functioning of the foot and can potentially limit the shock absorbing capacity of the arch. Though it’s almost impossible to find shoes without large toe springs, some minimalist running shoes or barefoot style shoes are lower in the front and flatten out easier.
No Built-In Arch Support
A structural arch gets its strength from the ends, not in the middle. In the case of the foot, the two ends of the arch are the heel and the toes. These are the parts of the foot that need to be in contact with the ground to support the foot.
Arch supports seem like the wrong way of supporting the foot because they prop the arch up from the middle. If you saw an arched doorway in a building you wouldn’t call up the architect who designed it to tell him he should have put more support in the middle!
The natural arch of the foot provides both support as well as shock absorption. Using artificial support can alter the foot’s ability to cushion impact forces. To some degree using an arch support closes off that space underneath the foot where muscles, nerves, and blood vessels pass. In some cases I suspect the position of the built-in arch of the shoe adds compressive stress to the heel.
Low Heel Height
Wearing a shoe with a raised heel is the same thing as standing on a ramp facing downhill all day. The result of this is adaptive shortening of the muscles in the calves and Achilles. A raised heel also tips your body forward. This forces the wearer to lean backward to stay balanced which then can place more weight on the heels. I look for relatively flat shoes, with little to no difference in height from the heel to the forefoot.
Making the switch. For someone used to wearing heavily structured, supportive shoes, the key is to transition slowly! The body needs time to adjust. A person used to walking barefoot at home may find the transition to be a little easier.
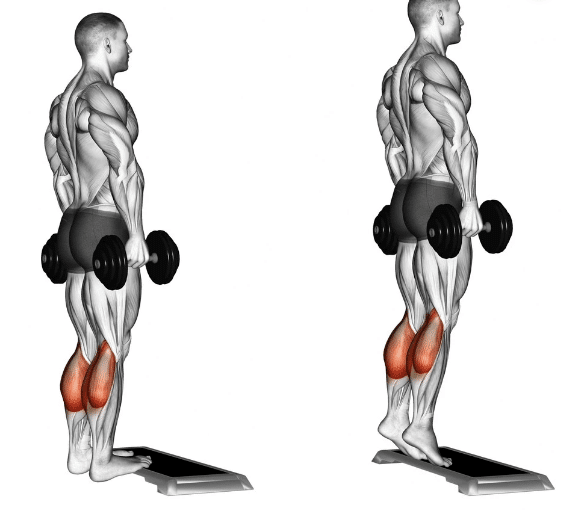
Step 5: Strengthen
Since plantar fasciitis is often associated with degeneration of the tissue in the foot, it makes sense that strengthening those tissues should be a priority. A recent study out of Denmark found a strength training program consisting of single-leg heel raises with a towel inserted under the toes resulting in better outcomes than a plantar fascia stretching program.
These results suggest getting the muscles in the underside of the foot some use should be a priority. This will naturally happen by increasing barefoot activity, but including some of the following exercises may help the process:
Foot Strengthening Exercises
- Short Foot Exercise: Try to form and hold an arch in the foot. Hold for 5 seconds, relax, and repeat (video)
- Foot Gymnastics: This can include any activity that requires foot dexterity. Some options are grabbing a pen with the toes, passing a pen back and for between your feet, picking up marbles, or stacking plastic cups. Imagination is the limit!
- Towel Curl: Spread a towel out on the floor and try to bunch it up by pulling it in with the toes but without moving the rest of your foot (video)
- Imaginary Beach: pretend you are gripping sand with your toes, picking it up, and then dropping it.
General Leg Strengthening
- Calf Raises: Raise up high on the toes and then lower down slowly. Focus on pushing through the big toe on the way up
- Toe Walking: Stand on the toes and walk 10-15 steps at a time keeping the heels off the ground
- Squats: Body weight squats are a great way to build leg strength and increase ankle flexibility
- Single Leg Balancing: Practice balancing on one leg to increase ankle and lower leg strength
- Hip Strengthening: Hip strengthening exercises can improve the mechanics of the foot
Step 6: Stretch
Hamstring Stretches:
There is some evidence that tight hamstrings, like tight calves, play a role in causing plantar fasciitis. I found the following stretches helpful when I had this injury.
Towel Stretch
Standing Stretch
Foot Stretches:
Stretching the foot is important for promoting flexibility and circulation, as well as adding stress to the tissue to encourage healing. These stretches bring the toes through a full range of motion. Many people find these helpful for making the first few steps in the morning less painful.
Plantar Fascia Stretch:
Toe Extensor Stretch:
Here is a video that shoes a fairly comprehensive stretching routine:
Massage
Massaging the calves and underside of the foot can promote tissue health, though the exact mechanisms involved are not yet understood. Two of the most commonly used self-massage techniques for plantar fasciitis are:
- Rolling a tennis or golf ball under the foot
- Using a foam roller to massage the calves–many runners swear by this (video)
Final Notes
It’s really difficult to make specific shoe recommendations because of the variability in styles that each brand makes. I tend to think the more structured a shoe is, the more likely it will interfere with the mechanics of the foot. I don’t think a complete switch to minimalist shoes is necessary. The guidelines in the article are a good starting point for what to look for, but I’ve come to realize there is no such thing as the “perfect” shoe. Finding something that’s comfortable is important, as well as understanding that there is very little evidence to suggest the support features built into shoes have any beneficial effects.
If an athlete’s heel pain just started, it’s not a bad idea for them to take a week or two off from your normal training. I also like the concept of “relative rest” which means substituting a new activity for the one aggravates the symptoms. The relative rest period is a good time to work on strength, flexibility, and mechanics in preparation for a gradual return to regular activity.
When the pain has persisted for several months (as is often the case with plantar fasciitis), I’ve found that activity is often better than rest. Overcoming the fear that activity will make the condition worse can also be an important part of the recovery.
If you’re ready to discuss your struggles with Plantar Fasciitis, speak to the team at Pivotal Motion! Our team provides tailored exercise physiology and physiotherapy Brisbane residents trust for their quality and effectiveness. Get in touch with us today on 07 3352 5116 or book your appointment now!